5 Operational Strategies to Improve Billing in Your Urgent Care
Enhance billing performance in urgent care with 5 operational improvements.

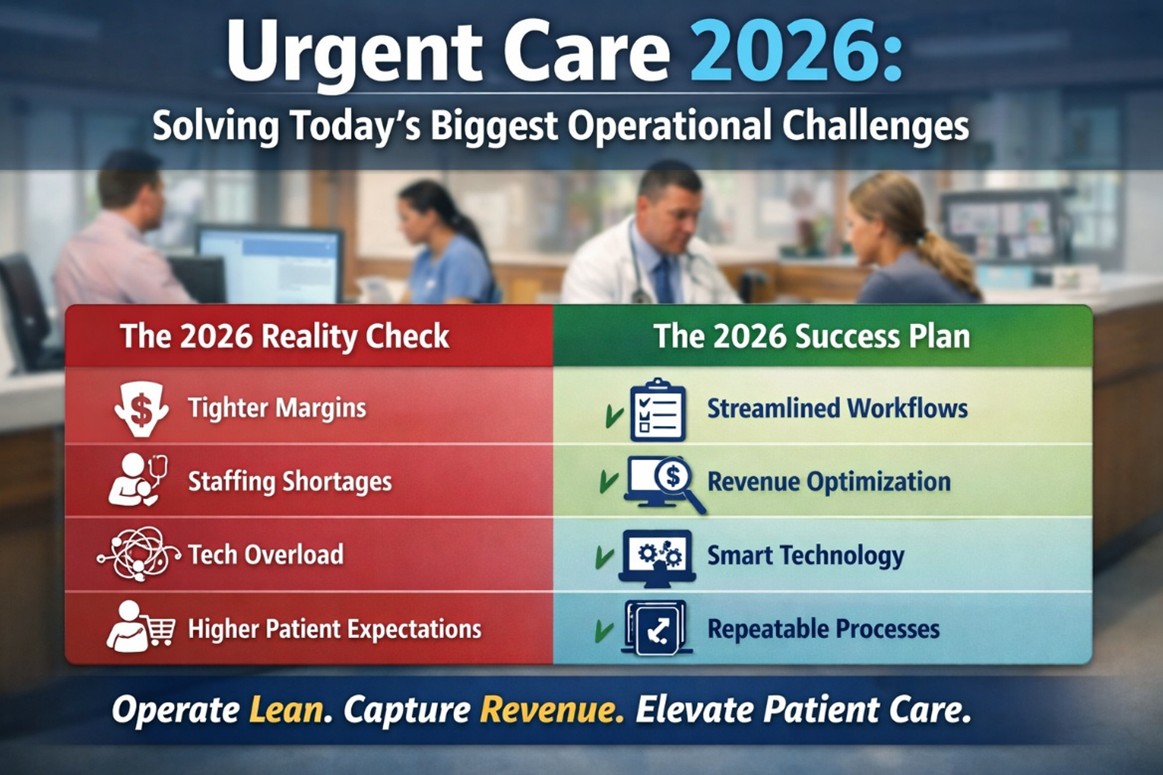
In today’s competitive urgent care environment, many operators focus on attracting more patients—while unknowingly leaving revenue on the table due to avoidable operational gaps. Poor documentation, eligibility errors, or sluggish chart closure can all slow down—or even halt—billing.
If you’re looking to improve your urgent care’s collections, the answer isn’t always “more volume.” Instead, fine-tuning your operations can lead to faster payments, fewer denials, and higher profitability.
Here are five operational improvements that can directly enhance your billing performance:
1. Streamline Front Desk Intake and Eligibility Verification
First impressions matter—and not just for patient satisfaction. Your front desk is the first line of defense for accurate billing.
Tips to implement:
- Use real-time eligibility tools integrated with your EMR
- Train staff to verify insurance and collect co-pays before the visit
- Standardize how demographics and insurance data are captured
Why it matters: Incorrect or missing insurance info is one of the top causes of claim rejections.
2. Close Charts Promptly
Unclosed or delayed charts mean delayed billing—and often forgotten charges.
Tips to implement:
- Set expectations for providers to complete documentation within 24–48 hours
- Use EMR dashboards to monitor open charts in real-time
- Provide incentives for timely chart closure
Why it matters: The longer a chart remains open, the more likely it is to result in missed revenue opportunities.
3. Standardize and Automate Coding
Coding errors can delay payment or lead to audits. Consistency and automation help reduce mistakes.
Tips to implement:
- Use EMR features that auto-suggest CPT and ICD-10 codes based on documentation
- Run weekly audits to catch under-coding or upcoding
- Provide regular training on common urgent care coding scenarios (e.g., laceration repairs, splints)
Why it matters: Correct coding ensures you're getting paid the full amount for the services you provide.
4. Track Denials and Rejections
Most urgent cares don’t realize how much revenue is lost through preventable denials.
Tips to implement:
- Set up a weekly denial report to identify trends (payer-specific, code-specific)
- Use a billing partner or in-house team to resubmit corrected claims quickly
- Categorize denials by root cause and address operational fixes (e.g., training, templates)
Why it matters: Understanding the “why” behind denials helps you fix problems at the source.
5. Implement Daily or Weekly Billing Huddles
Proactive communication between clinical, billing, and front desk staff keeps your revenue cycle tight.
Tips to implement:
- Use quick 15-minute huddles to review issues like missing documentation or chart errors
- Share wins and losses to create accountability
- Identify bottlenecks and fix them in real time
Why it matters: Operational alignment is critical for consistent cash flow.
Final Thoughts
Billing is not just a back-office issue — it’s a full-team effort that begins at patient check-in. By aligning your operations with your revenue cycle, you can reduce delays, improve cash flow, and ultimately boost the profitability of your urgent care.
Want to see how technology can support these improvements? Contact us at UrgentIQ to learn how our EMR platform is built specifically for urgent care operations. Sales@urgentiq.com
More blog posts to read
Prefer to send an email? Send us your request at sales@urgentiq.com, and we'll coordinate with you directly.
We're thrilled that you're interested in joining us. Please fill out the form below to get started on your journey with UrgentIQ.


.png)