Medicare Telemedicine Updates: What Urgent Care Centers Need to Know Amid the Government Shutdown
Medicare telehealth is extended through 2025, but urgent care centers must prepare for policy shifts and reimbursement risks.
Medicare Telemedicine Updates: What Urgent Care Centers Need to Know Amid the Government Shutdown
Introduction
Telemedicine has become an operational lifeline for urgent care centers, extending access, improving throughput, and enabling continuity during off-hours or peak volume days.
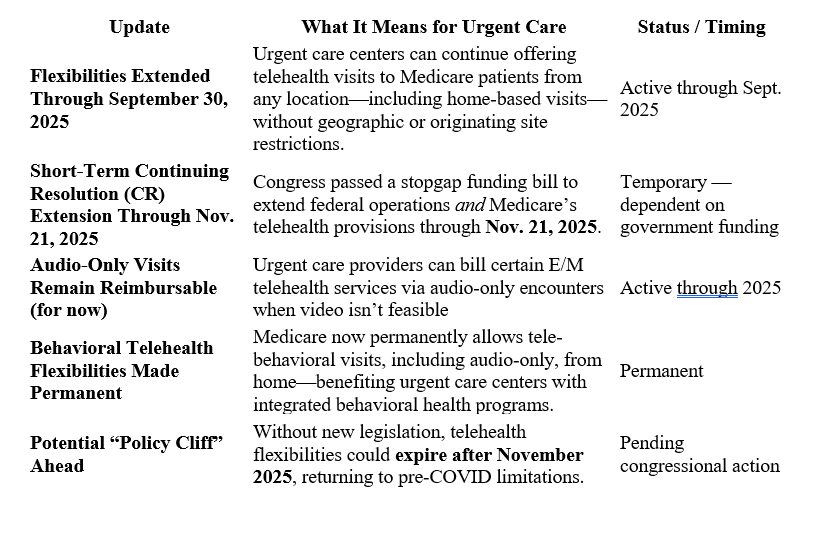
Since the COVID-19 pandemic, Medicare telehealth flexibilities have allowed urgent care providers to serve patients remotely—whether from their homes, rural communities, or senior living facilities. But those flexibilities were never permanent.
Today, as the federal government shutdown collides with pending Medicare legislation, urgent care operators face mounting uncertainty around reimbursement stability, billing rules, and future telehealth viability.
Let’s break down the current status, what’s at stake, and what action steps you should take to protect your center’s revenue stream and operational integrity.
Medicare Telehealth Coverage: The Current Landscape
How the Government Shutdown Impacts Urgent Care Telehealth
The current federal government shutdown poses real-world risks for urgent care centers that offer telemedicine services.
1. Legislative Delays Could Stall Telehealth Permanency
Bills like the CONNECT for Health Act and Telehealth Modernization Act are designed to make telehealth coverage permanent—but all legislative activity is paused during the shutdown.
What this means: Urgent care operators should not assume telehealth coverage is “locked in.” The timeline for permanent Medicare reform is now uncertain.
2. CMS Administrative Slowdowns
During a shutdown, CMS operates with limited staff. This delays the release of guidance memos, billing clarifications, and code updates that urgent care billing teams depend on.
What this means: Expect slower updates for 2026 fee schedules, modifier clarification (POS 10 vs POS02), and telehealth parity notices.
3. Possible Payment Processing Delays
While Medicare payments continue for now, extended shutdowns can cause delays in claims adjudication and reimbursements across all services and payers, especially for newer telehealth codes.
What this means: Urgent care centers should monitor cash flow closely and maintain reserves or flexible financing for short-term interruptions.
4. Private Payer and State Medicaid Uncertainty
Commercial payers and Medicaid programs often mirror Medicare’s telehealth coverage timelines. If Medicare freezes, they may pause or stagger updates.
What this means: Be prepared for inconsistencies in payer rules for telemedicine visits between October and December cycles.
5. Operational and Compliance Risks
Reduced CMS communication can result in compliance confusion—especially regarding place-of-service codes, telehealth modifiers, and documentation for audio-only visits.
What this means: Urgent care billing staff should flag potential discrepancies early and maintain thorough encounter documentation.
Strategic Playbook for Urgent Care Operators
In today’s volatile reimbursement environment, urgent care executives and administrators should act decisively to maintain telehealth continuity and compliance.
1. Perform a Telehealth Financial Impact Audit
Quantify how much of your monthly revenue is tied to Medicare telehealth and telephonic visits. If those codes were disallowed tomorrow, what would your cash flow look like? Also consider the impact if other commercial carriers were to follow suit with similar Medicare changes.
2. Build Hybrid Visit Workflows
Create flexible scheduling protocols that can toggle between telehealth and in-person visits seamlessly. This minimizes patient disruption if coverage shifts mid-cycle.
3. Train Billing and Front Desk Staff
Ensure staff understand the correct codes and modifiers (e.g., 93 for audio-only, POS 10 for home-based telehealth). Consistency here protects revenue and compliance.
4. Monitor CMS and Advocacy Channels
Follow updates from CMS, the Urgent Care Association (UCA), and the American Telemedicine Association (ATA). Encourage your billing partner to share real-time alerts.
5. Communicate with Patients Proactively
Prepare templated messages or discharge instructions explaining that coverage for telehealth services remains active for now but could change after November 2025. Transparency builds trust.
6. Engage with Vendors and EMRs
Ensure your EMR platform—like UrgentIQ—is optimized for rapid code changes, hybrid scheduling, and automated claim logic updates. Agility in your tech stack is your best defense.
The Broader Picture: Urgent Care’s Role in Telehealth Evolution
Urgent care has become the front line of accessible, on-demand medicine. As policymakers debate telehealth’s long-term status, urgent care centers are living proof that virtual care complements—not replaces—physical medicine.
The operational flexibility that urgent care embodies—fast, adaptable, patient-centered—positions it to lead the charge in integrating hybrid models that combine convenience with clinical rigor.
But sustaining that role depends on stable reimbursement, clear policy, and modern EMR infrastructure capable of adapting overnight to regulatory shifts.
Final Thoughts
Medicare’s telehealth coverage remains extended—for now. But the government shutdown has frozen legislative progress and delayed CMS operations, leaving urgent care operators in a state of watchful waiting.
The best defense is preparation:
- Audit your exposure
- Train your team
- Stay nimble with your tech
- Communicate proactively
Urgent care’s strength has always been adaptability. Navigating telehealth uncertainty is simply the next frontier of that legacy.
To learn more about how the right EMR can help you prepare to delivery telehealth services within the current and future guidelines, contact sales@urgentiq.com
More blog posts to read
Prefer to send an email? Send us your request at sales@urgentiq.com, and we'll coordinate with you directly.
We're thrilled that you're interested in joining us. Please fill out the form below to get started on your journey with UrgentIQ.